This fall, the United States Supreme Court will hear arguments in California et al. v Texas et al. The Court will decide whether the Affordable Care Act’s (ACA’s) “individual mandate” remains constitutional even though Congress has zeroed out the tax penalty for not maintaining health insurance. The Court also will decide whether, should the individual mandate be deemed unconstitutional, Congress, in setting the tax penalty at zero, actually intended to repeal the entire law. Repealing the Affordable Care Act (ACA) would eliminate the Medicaid expansion for low-income adults, subsidized Marketplace health insurance, and the Community Health Center Fund. Thus, at a time when the nation is confronting the worst public health emergency in a century, health care for tens of millions of people is on the line. A new blog, by our colleagues at the Geiger Gibson/RCHN Community Health Foundation Research Collaborative, looks at the impact on community health centers and the patients they serve if the Affordable Care Act is repealed. The authors find that eliminating Medicaid and Marketplace coverage would result in a $3.5 billion loss of health center revenue nationally in a single year, which translates into closure of 1,432 service delivery sites, and reductions of 3.4 million patients, 14.2 million visits, and nearly 29,000 full-time equivalent staff. These estimates understate the total impact of ACA repeal, since they do not include the revenue impact of eliminating the Community Health Center Fund, which is also at risk.
Read the blog, “If the Affordable Care Act is Repealed, What Would Be the Impact on Community Health Centers and the Communities They Serve?” on the GW Health Policy and Management Matters Site.
__________________________________________________________________________________________________________________________
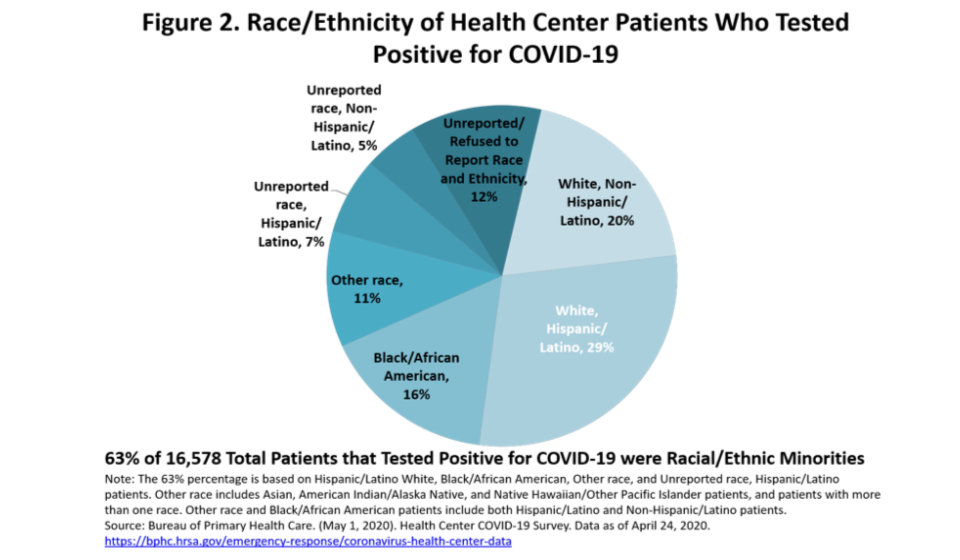
Data Note: COVID-19 Survey Update
Our latest data note updates previous findings on the impact of COVID-19 on community health centers. The data note is based on survey data collected by HRSA, as reported for April 24, 2020. Compared to their pre-COVID-19 visit volume, health centers reported a decrease in visits of 47 percent percent nationally, with health centers in 23 states reporting a decline in total visits of at least 50 percent. In five states, at least 75 percent of visits conducted in the week prior to the survey were telehealth or telephonic visits. The pandemic has forced the temporary closure of 1,779 sites, or approximately one in seven sites nationally. Nationally, health centers reported that 54 percent of patients tested for COVID-19 were racial and/or ethnic minority patients, and among all health center patients who tested positive for COVID-19, nearly 2 of 3 (63 percent) were identified as racial/ ethnic minorities.
Read the data note: Key Updates from the Health Center COVID-19 Survey: Week 4
__________________________________________________________________________________________________________________________
What Can We Learn from the Telehealth Experience of Community Health Centers During the COVID-19 Pandemic?
As the COVID-19 pandemic continues to ravage communities across the country, the availability and utilization of telehealth has taken on greater importance. Last week, survey data from the Health Resources and Services Administration (HRSA) indicated that, on average, 54 percent of health center visits were being conducted virtually. A new data note explores the use of telehealth by community health centers, and outlines the substantial barriers to telehealth adoption related to reimbursement, up-front investment, and staffing. While telehealth has the potential to substantially improve access to care in medically underserved rural and urban communities in both the near and long term, these barriers must be addressed in order for its potential to be realized. Health centers will be an important bellwether of progress as telehealth policy and implementation unfold. The data note was written by Rebecca Morris, James Hernandez, Sara Rosenbaum, Feygele Jacobs, Peter Shin and Jessica Sharac.
Read the data note: What Can We Learn from the Telehealth Experience of Community Health Centers During the COVID-19 Pandemic?



