On August 4, 2020 Missouri became the 39th state (including DC) to adopt Medicaid expansion, and the 6th state to have done so through a voter initiative. Prior research has documented a significant and measurable relationship between the strength of community health centers and their location in ACA Medicaid expansion states. A new data note examines the potential impact of Medicaid expansion, which is expected to be fully operational by July 2021, on Missouri’s community health centers and their patients. Researchers estimate that expansion can be expected to insure an additional 36,000 to 42,000 health center patients and to increase health center revenue statewide by $34 to $40 million, or 6 to 7 percent. These coverage gains can be expected to expand both the volume and scope of services that health centers are able to provide or arrange for by generating more operating revenue, which in turn will permit health centers to strengthen care capacity. The state’s health centers can be expected to care for an additional 36,000 to 43,000 patients – both insured and uninsured – as services expand overall, and to provide 133,000 to 156,000 more visits. The analysis suggests that Missouri’s Medicaid expansion will produce the same measurable, beneficial community-wide effects seen in community health centers in expansion states across the nation. As part of the diverse Healthcare for Missouri coalition, Missouri Primary Care Association members played a central role in educating the public about the Medicaid expansion effort through a campaign that generated more than 1 million Get Out The Vote (GOTV) phone calls, ultimately overcoming – by some 82,000 votes – a strong effort by opponents to defeat the measure.
The data note is authored by researchers at the Geiger Gibson/RCHN Community Health Foundation Research Collaborative at the George Washington University Milken Institute School of Public Health (Milken Institute SPH).
Read the data note, “Missouri’s Historic Medicaid Expansion Will Produce Major Gains for that State’s Community Health Centers, their Patients and the Communities They Serve”
__________________________________________________________________________________________________________________________
NHCW Recap
We celebrated this year’s National Health Center Week (NHCW) amidst a global pandemic that has required extraordinary innovation, effort and resilience. This year’s theme, “Community Health Centers: Lighting the Way for Healthier Communities Today and in the Future” honored front line providers, staff, and beloved patients who have lost their lives to COVID-19. As we continue to face this unprecedented health crisis, health centers remain at the forefront, responding both to the crisis and the needs of their communities.
This year, we joined our colleagues in virtual celebrations across the country. With the help of technology it was a quick trip to Mary’s Center in Washington DC. Founded in 1988, Mary’s Center has grown from a small basement clinic that served 200 women a year to a comprehensive community health center serving men, women and children of all ages. Led by President and CEO Maria S. Gomez, RN, MPH, the center’s NHCW Virtual Town Hall allowed us a glimpse into the difficult challenges the Mary’s Center community has faced during the pandemic – including job losses and wage cuts, food and housing insecurity, and disruption to education – and the emotional toll and impact of the crisis on everyday life. We also had the opportunity to hear about the health center’s remarkable work to ensure continued care and access for their community. Through telemedicine, the center provided medical, dental, behavioral health, social services, nutrition and health education services. In addition, the center arranged home visits to ensure elderly patients got the care they need, provided 200 Chrome Books to under-resourced families, and continues to advocate for accessible internet in their county. Learn more about Mary’s Center.
Closer to home, we stopped by Ryan Health in New York City: Founded in 1967, Ryan Health offers the full range of primary care, vision, dental, behavioral health, women’s and children’s health in diverse neighborhoods throughout the borough of Manhattan, including the Lower East Side, Hell’s Kitchen, Manhattan Valley, Harlem and Washington Heights. Ryan Health’s virtual workshop series for NHCW highlighted key health and social services to help neighbors cope during the pandemic. We joined “Diabetes: Get up and get moving” a workshop focused on diabetes education. Participants learned simple, accessible ways to incorporate more activity into their lives, without the need for a gym. The session, presented by certified Diabetes Educator Amy Zarrow, and a fitness instructor, ended with a mood-boosting at-home yoga and exercise demonstration, empowering participants by providing important tools to take care of their health. Learn more about Ryan Health’s comprehensive primary and specialty services via their website.
Finally, we visited Urban Health Plan Inc. located in the Bronx. Founded by the late Dr. Richard Izquierdo in 1974, it now provides comprehensive primary and specialty health care services to the Hunts Point, Mott Haven and Morrisania sections of the Bronx, as well as Central Harlem and Corona, Queens. Urban Health Plan offered a virtual back-to-school video series with pediatricians Dr. Rose Taveras, Dr. Shamiza Ally, Dr. Viju Jacob, Dr. Gladys Banegas and social worker Janely Perez, who provided meaningful suggestions on how to help children transition back to school as the pandemic continues. We tuned into a nutrition segment, “Cooking with Karla” where we learned easy, practical ideas for preparing a nutritious school lunch from Chef Karla Giboyeaux. Watch the video to learn more.
As COVID-19 surges, health centers across the country have stepped up to serve their communities. Community health centers have tested more than 2.6 million patients for COVID-9 virus since April, and have endured sustained losses in staffing, site closures, gaps in the supply of PPE and ongoing visit declines driving substantial revenue losses. Without ongoing financial support, health centers’ ability to sustain operations and fully restore primary care capacity could be significantly affected, and continued advocacy and outreach are essential to ensure that community health centers get the support and funding they need. We thank the National Association of Community Health Centers for their leadership and applaud the work of our community health center colleagues for their dedicated service to all members of the community, regardless of their insurance status or ability to pay, 52 weeks each year.
__________________________________________________________________________________________________________________________
Learning Opportunities at Upcoming Virtual Conferences
The Association of Clinicians for the Underserved (ACU) will hold its Virtual Conference from September 14-18, 2020. Colleagues Paul Melinkovich, MD, FAAP, Senior Clinical Advisor, RCHN CHF and Seth Doyle, Director of Strategic Initiatives, Northwest Regional Primary Care Association (NWRPCA) will be presenting a workshop “Supporting Community Health Workers to Enhance Effectiveness in Advanced Primary Care Settings,” on Tuesday September 15, at 10:00 AM – 12:00 PM Eastern Time.
RCHN CHF population health program colleagues will also be presenting a session at the Community Health Centers of Arkansas (CHCA) Virtual Annual Conference, “Teams: Leaping Boundaries-Expanding Health – Social Determinants of Health”, Thursday Sept 17, at 4:00 PM – 5:00 PM Central Time. The session will be hosted by David Stevens, MD, FAAFP, Senior Clinical Advisor, RCHN CHF and Research Professor, Milken Institute, School of Public Health, George Washington University, joined by our colleagues Talya Hellman, MPH, Manager, Planning and Development, and Nicole Lee, LCSW, Director of Care Coordination, both at Access Community Health Network (IL).
__________________________________________________________________________________________________________________________
New from KFF – Community Health Centers and Medication-Assisted Treatment for Opioid Use Disorder
As the country struggles to respond to the coronavirus pandemic, emerging evidence suggests drug overdoses are increasing sharply, with an estimated 18% increase in overdoses since the start of stay-at-home orders in March through May 2020. Community health centers play a significant role in addressing the ongoing opioid crisis, with the capacity to screen, treat, refer, and provide supportive services such as case management to patients experiencing opioid use disorder (OUD); CHCs have become a major source of medication-assisted treatment (MAT), the standard of care for those with OUD. This issue brief from Kaiser Family Foundation presents findings from a 2019 survey of community health centers on activities related to the prevention and treatment of OUD, with a focus on MAT, to assess services and capacity prior to the recent surge in need. Key findings indicate that:
- As of 2019, an increased share of health centers were providing MAT services (64%, compared to 48% in 2018).
- Most health centers that provide MAT offer multiple treatment options for patients experiencing OUD.
- Health centers face many challenges meeting the high demand for OUD treatment, including capacity and provider shortages.
The authors find that targeted federal grants from 2016 to 2019 helped health centers bolster MAT programs and establish new ones, although health centers continue to rely heavily on Medicaid to sustain MAT programs and services long-term. However, the high cost of providing MAT services remains a barrier in both Medicaid expansion and non-expansion states, and these barriers will likely remain even as the coronavirus pandemic poses new challenges for health centers’ finances and capacity to provide OUD services.
The brief was authored by researchers from the Geiger Gibson/RCHN Community Health Foundation Research Collaborative at Milken Institute School of Public Health, George Washington University (GW) and the Kaiser Family Foundation. Additional funding support was provided by the RCHN Community Health Foundation.
The brief is available on the KFF site.
__________________________________________________________________________________________________________________________
More to Read and Watch
- The Funders Forum on Accountable Health has released, “Building Equity and Community Accountability into Pandemic Response and Recovery: A Proposal to Create Response and Resilience Accountability Councils.”
- The Puerto Rico Primary Care Association/ ASPPRR has issued, “Puerto Rico PCA 4-Part Learning Conversation Series” – ASPPR Covid-19 Best/Promising Practices, detailing their series for CHC leadership and care managers. This free educational series offered participants a continuous cohort-based learning experience, with 39 sessions related to Human Resources & Finance; Mental Health and Substance Use; Emergency Response, and Women’s Health.
- Data Note – Key Updates from the Health Center COVID-19 Survey (Week #19): Average Turn-Around Times for COVID-19 Viral Test Results and Capacity Measures Reported by Community Health Centers Improved this Week, but Remain Substantial, part of an ongoing series from the Geiger Gibson RCHN Community Health Foundation Research Collaborative.
- Also from the GG/ RCHN CHF Collaborative, a Data Note: As COVID-19 Surges, Community Health Centers Face Near-Term and Long-Term Funding Instability.
- The CHroniCles Beat: Amidst a Pandemic, Agricultural Workers Toil and Community Health Centers Adapt and Innovate, checks in with colleagues at National Center for Farmworker Health and New York’s Oak Orchard Health and Finger Lakes Community Health to learn about the impact of COVID-19 on agricultural communities.
- WIVB-4 News recently visited Oak Orchard Health and recorded a related feature story, Local Health Center Ahead of the Curb in Fighting Coronavirus.
__________________________________________________________________________________________________________________________
CHroniCles Feature Albums
All over America, community health centers were founded by visionary local leaders, activists and advocates who saw a pressing need for health care services and committed to meeting those needs. Together with early health center staff and community-based board leadership, they created the foundation not just for local services, but for the comprehensive community health center system of care that we know today. Follow our Facebook page to view more feature albums. And there’s still time to participate in our raffle, extended to Labor Day.
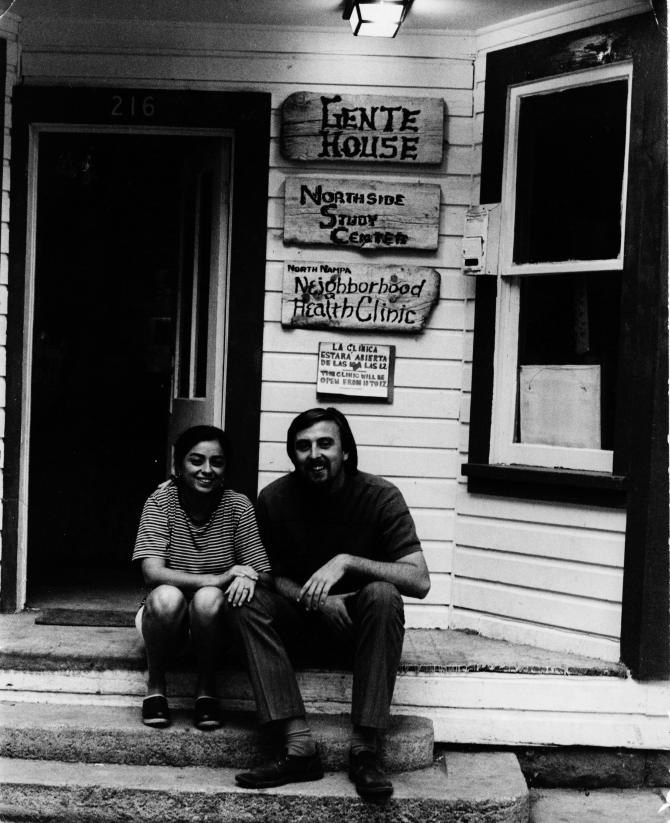
Founders Terry Reilly and Rosie Delgadillo Reilly sit on the front steps of Gente House, the original home of the neighborhood clinic that became Community Health Clinics, Inc. and was later renamed the Terry Reilly Health Services in tribute. (Nampa, ID)
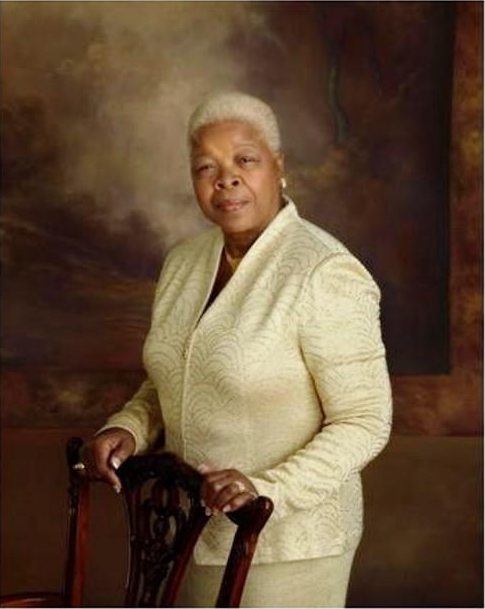
Ms. Betty Jean Kerr RN, BSN, PNP, MA joined the People’s Health Center as CEO in 1977 and turned the volunteer-led storefront free clinic into a comprehensive network. Upon her retirement after more than 30 years of service, the health center was renamed the Betty Jean Kerr People’s Health Center in her honor. (St. Louis, MO)
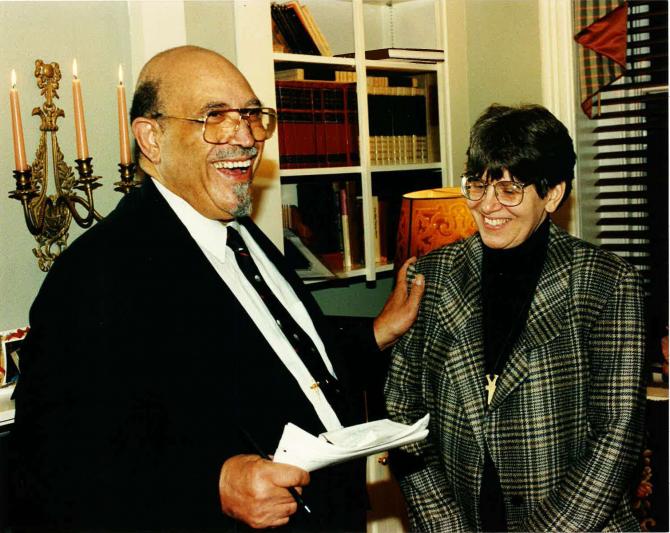
Dr. Janelle Goetcheus and Dr. Jesse Barber founded Washington D.C.’s Health Care for the Homeless Project (HCHP) in 1985. The organization expanded to provide comprehensive care to all residents of the District and is now known as Unity Health Care. (Washington DC)

Hudson River HealthCare, Inc. was founded more than 45 years ago as the Peekskill Area Ambulatory Health Center, when a group of four women – the “Founding Mothers” Mary Woods, Willie Mae Jackson, Pearl Woods, and Reverend Jeannette Phillips – worked with community members and religious leaders to address the need for affordable health care in Peekskill, one of the poorest cities in N.Y.’s Hudson River region. (Peekskill, NY)

Ms. Doris Ison compelled doctors and legislators to create a health care center in South Miami Dade to provide care to the area’s local Black residents, who were not welcome at the area’s hospitals. The health center, which began 1971 in two meager trailers, is now Community Health of South Florida, Inc. (Miami, FL)



