Community Health Worker Institute Will Reimagine Role of CHWs in CHCs and Communities
Seattle-based Northwest Regional Primary Care Association (NWRPCA), which represents community health centers in Alaska, Idaho, Oregon, and Washington will be launching a new Community Health Worker (CHW) Institute, supported by a major grant from the RCHN Community Health Foundation.
CHWs are an invaluable frontline resource, and will prove essential for developing a more resilient future as the healthcare system rebuilds following the COVID-19 pandemic. “The global pandemic has laid bare some of the things we need to do better in our current health care system,” said NWRPCA CEO Bruce Gray. “And it all comes back to rethinking not a better illness system, but how to prevent disease and improve people’s health.”
Evidence shows that CHWs are uniquely suited to serve as liaisons between health care, social services, and the community. They facilitate access to services and improve the quality and cultural competence of service delivery, often working to address social determinants of health including food insecurity, housing conditions and adverse community environments.
The CHW Institute will build on NWRPCA’s ongoing leadership in training and technical assistance, and serve as a training, TA, and resource hub to help community health centers more effectively engage, support and integrate CHWs into health center care teams. NWRPCA aims to deepen the understanding of the role of community health workers within medical homes and the health care system, promote greater recognition of their impact on addressing the social determinants of health, and provide access to high-level training to help build capacity. It will also promote ways to leverage the CHW model to strengthen the health care system and promote sustainable policy while advancing public health.
Dr. Patrick Luedtke, Senior Public Health Officer of Lane County Oregon and current NWRPCA board chair, explained “Engaging at the community level is the key to improving health. The COVID-19 vaccine will travel at the speed of trust and community health workers are key to developing trust.”
To help develop the Institute’s work, NWRPCA will engage partners with expertise in public health, community health worker training and professional development.
The development of the CHW Institute builds on a recent NWRPCA initiative supported by RCHN Community Health Foundation to better understand how CHWs are engaged in and might enhance behavioral health-primary care integration in community health center-based settings.
Read the press release.
__________________________________________________________________________________________________________________________
Data Note – How the COVID-19 Pandemic Has Intensified the Impact of the Public Charge Rule on Community Health Centers, their Patients, and their Communities
A new data note discusses the heightened impact of the public charge rule on community health centers, patients and communities resulting from the COVID-19 pandemic.
The public charge rule represents a serious threat for immigrants who seek permanent U.S. residency status. Of major concern is both the rule’s impact on Medicaid, and whether immigrants would avoid health care itself. Research has documented the rule’s significant chilling effect, both on those directly subject to its terms as well as on their families, including citizen children, with the sanctions expected to have a substantial effect on health center revenue and care capacity. Prior estimates by the authors found that between 165,000 and 495,000 Medicaid patients at community health centers could be expected to lose coverage, translating to a decline in the capacity to serve between 136,000 and 407,000 health center patients nationally, and revenue declines ranging from $164 million to $493 million as a result of the Medicaid coverage drop.
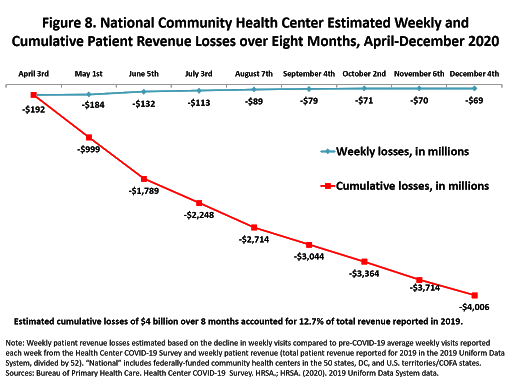
Since that time, as a direct result of the COVID-19 pandemic, community health centers have lost an estimated $4.006 billion in cumulative patient revenue over eight months, or 13 percent of all 2019-reported revenue. At the same time, the pandemic has demanded a major increase in care capacity, especially for the worst-hit populations, who tend to reside in impoverished communities and to include large numbers of immigrants. Funding to offset the effect of the pandemic has been inadequate. With no additional federal COVID-19 financial relief yet committed, health centers will be unable to restore operational capacity to pre-pandemic strength. Thus, the public charge rule becomes a matter of even greater concern both because of the direct threat it poses to community health when care is most needed, and because of its spillover financial and operational effects on community health providers struggling to care for their communities.
The data note was produced by the Geiger Gibson/RCHN Community Health Foundation Research Collaborative.
Read, “How the COVID-19 Pandemic Has Intensified the Impact of the Public Charge Rule on Community Health Centers, their Patients, and their Communities”
__________________________________________________________________________________________________________________________
The Status of Community Health Centers in the Midst of the Worst Phase of the COVID-19 Pandemic
With the nation facing the worst phase of the COVID-19 pandemic to date, and on the cusp of a broad-based vaccination campaign, our latest data note reports updated data trends for the eight-month period from April 3 through December 4.
Community health centers have tested more than 6.2 million patients for COVID-19 virus over the eight-month period, with the number of patients tested for the COVID-19 virus this week (335,139) reaching the highest level reported over eight months. In the aggregate, a total of 744,142 health center patients have tested positive for the COVID-19 virus, accounting for 5.2 percent of cases nationally, or 1 in 19 of all U.S. cases.
With weekly health center visits consistently lower than before the pandemic and no additional federal COVID-19 financial relief yet committed, the pandemic has taken an enormous financial toll on health centers, resulting in an estimated $4.006 billion in cumulative patient revenue losses over eight months, or nearly 13 percent of total health center revenue reported nationally in 2019. These findings underscore the continued need for the expansion of health center testing resources, and the support for full participation of health centers in COVID-19 vaccine distribution plans. It is estimated that nearly half (47 percent) of health center patients would qualify for Phase 1 COVID-19 vaccination because they are adults of advanced age or with underlying health conditions that put them at higher risk of serious COVID-19 illness. In the face of deep financial losses, continued financial uncertainty, and as the nation faces both the flu season and increased coronavirus cases, the future of our nation’s health centers should be a cause for both deep concern and renewed long-term support.
The data note was produced by the Geiger Gibson/RCHN Community Health Foundation Research Collaborative.
Read the date note, “Key Updates from the Health Center COVID-19 Survey (Week #36): The Status of Community Health Centers in the Midst of the Worst Phase of the COVID-19 Pandemic”
__________________________________________________________________________________________________________________________
Policy Webinar Series: Health Policy in the New Administration
The health policy world will look quite different under the next President. The Geiger Gibson Program is hosting a special four-part series, beginning immediately after the inauguration, exploring federal health policy issues pertinent in the new administration, starting January 21, 2021, right after the next President is sworn in. Webinars will be hosted by Sara Rosenbaum, JD, the Harold and Jane Hirsh Professor of Health Law and Policy at the George Washington University, featuring expert presenters from within GW and around Washington, DC. Additional commentary will be provided by community health center leaders including Paloma Hernandez (Urban Health Plan, NY), Anne Kaufmann Nolon (Sun River Health, NY), Anita Manoian, (Yakima Neighborhood Health, WA), and Michael Taylor (Cornell Scott Hill Health Center, CT).
Presenters Include:
Katherine Hayes, J.D. – Director of Health Policy, National Bipartisan Policy Center
Leighton Ku, PhD, MPH – Professor and Director, Center for Health Policy Research, Milken Institute SPH at the George Washington University
Jocelyn Guyer, M.P.A. – Managing Director, Manatt Health
Topics will include:
The Biden administration’s blueprint for action – what does it mean for health centers and their communities
Insuring all low-income people – where is the administration headed?
How will reducing health disparities guide administration policymaking?
Health policy and immigrant health
Dates: Thursday January 21, Tuesday February 2, Tuesday February 16, Tuesday March 2
Time: 12:00 noon to 1:00 PM EST
Cost: $300 for the 4-part series
Registration: Register here
__________________________________________________________________________________________________________________________
The CHroniCles Beat: CHCs on the Frontlines of the Opioid Crisis During the COVID-19 Pandemic
America’s opioid epidemic has had a huge impact on the well-being of individuals and communities across the country, and 20 years into the epidemic there is a growing need for services. The COVID-19 pandemic has exacerbated an already tenuous situation for many people. Reports from national, state, and local media all indicate that opioid and drug-related mortality have increased since the pandemic started. In this CHroniCles Beat blog, we checked in with colleagues at Fenway Health (MA) and Central City Concern (OR) to learn about the programs and strategies they’ve developed to tackle the opioid crisis, and how they’ve addressed the unique challenges brought about by the COVID-19 pandemic.
Read, “CHCs on the frontlines of the opioid crisis during the COVID-19 pandemic”

Photo courtesy of Central City Concern (OR).
__________________________________________________________________________________________________________________________
We wish our community health center colleagues a safe, happy and healthy holiday!



