CHC’s Pandemic Experiences by State Medicaid Expansion Status: Reported Differences in COVID-19 Vaccination Rates and Weekly Visit Declines
Throughout the COVID-19 pandemic, case rates, vaccination rates, and COVID-19 policies have varied broadly across the US. Similarly, community health centers’ experiences have varied widely by state, underscoring the need for stable and sustainable resources to support the needs of the patients and communities served by our nation’s health centers. With rising unemployment and the related loss of employer-based coverage, and with some pandemic-era policies sunsetting, the availability of Medicaid coverage and thus the status of state Medicaid expansion is of heightened importance. Our latest report presents an analysis of grantee-level data from HRSA’s COVID-19 survey for the period April 2020 to the end of May 2021, to explore how rates of weekly visits and COVID-19 immunizations varied by state and by Medicaid expansion status.
While visits to community health centers declined sharply across all health centers, the losses were greater among health centers in non-expansion states, with health centers in those states reporting average losses in weekly visit volume of 55 percent in April 2020, compared to 51 percent among health centers in Medicaid expansion states. Recovery has also been slower: just over a year later, in May 2021, weekly visit volume at health centers in Medicaid expansion states had recovered to 93 percent of pre-pandemic levels, while health centers in non- expansion states reported weekly visit volume at 84 percent of pre-pandemic levels, fully 16 percent below pre-pandemic activity. These findings suggest both better patient access and greater service utilization, and as a result, more patient revenue flowing to expansion state health centers.
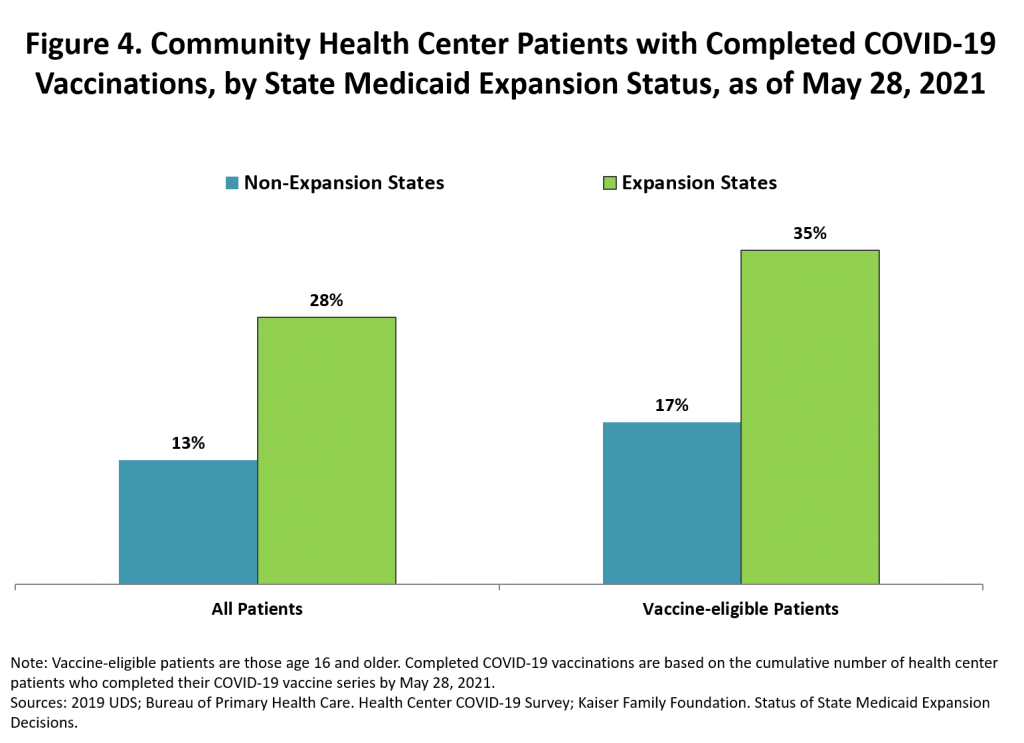
Community health centers in Medicaid expansion states also reported higher rates of completed patient COVID-19 vaccinations (28 percent) than those in non-expansion states (13 percent). Among vaccine-eligible adult patients, completed COVID-19 vaccinations was more than twice as high (35 percent) in expansion-state health centers compared to those in non-expansion state centers (17 percent).
As the nation begins to recover while addressing the uncertainties of the pandemic, the analysis suggests that health centers in non-expansion states, with fewer Medicaid-enrolled patients and fewer visits, may face a more difficult financial recovery. The pandemic’s disproportionate impact on low-income households, combined with community health centers’ essential role in serving low-income communities, underscores the importance of providing adequate funding to facilitate an equitable and robust COVID-19 response.
The data note was produced by the Geiger Gibson/RCHN Community Health Foundation Research Collaborative at Milken Institute SPH.
__________________________________________________________________________________________________________________________
Policy Issue Brief: Asian Patients Confront Multi Pandemics: Racism, Immigration, and COVID-19
A new policy issue brief entitled, “Asian Patients Confront Multi Pandemics: Racism, Immigration, and COVID-19” from the Association of Asian Pacific Community Health Organizations (AAPCHO) looks at how the COVID-19 pandemic, changing federal immigration policies including public charge and the associated “chilling effect,” and the rise in anti-Asian hate incidents have impacted Asian Americans and Asian immigrants.
The brief highlights the challenges of the simultaneous and ongoing multi pandemics – racism, immigration, and COVID-19 – confronting the Asian American and immigrant community. It describes the vital role community health centers have played in supporting community members, and outlines action recommendations for federal policy makers. Underscoring the significant health and mental health impacts, the brief emphasizes the need for robust resources to support trusted messengers, like health centers, that are critical to provide community-oriented solutions to address these challenges.
The data and recommendations are based on findings from an in-language survey conducted by the Kaiser Family Foundation (KFF) administered to more than 1,000 people served by four AAPCHO member community health centers – Asian Health Services (Oakland, CA), HOPE Clinic (Houston, TX), International Community Health Services (Seattle, WA) and North East Medical Services (San Francisco, CA). The policy brief was supported by the RCHN Community Health Foundation.
__________________________________________________________________________________________________________________________
Improving Data Quality and Capacity – The “D2 Project”
In 2019, in conjunction with Puerto Rico’s primary care association, Asociación de Salud Primaria de Puerto Rico, Inc. (ASPPR), and its affiliate, Puerto Rico Primary Care Association Network (PR PCAN), RCHN Community Health Foundation developed a project to support the development and reinforcement of a robust data culture in Puerto Rico’s community health centers. The project, known as D2, focused on two broad areas. The first was a data quality assessment to identify strengths, weaknesses, and variations in data collection and documentation practices among participating health centers. The second area of activity was to develop sample analytics and dashboards, demonstrating their benefit in clinical, financial, and operational decision-making. In collaboration with a pilot group of health centers, the D2 project was completed in 2021. The approach, key findings and recommendations are encompassed in the report, which emphasizes the need for data quality practices to ensure that available data becomes a key strategic asset that ultimately serves to improve the quality of health center services. Congratulations to ASPPR for shepherding this important initiative.
Read the D2 Project final report.
View related PowerPoint.
__________________________________________________________________________________________________________________________
In the News
Congratulations to community health center colleagues featured in the latest Crain’s New York Business “Notable in Health Care” 2021 for this well-deserved recognition: Dr. Neil Calman (The Institute for Family Health), Kaushal Challa (Charles B. Wang Community Health Center), Rose Duhan (CHCANYS), Sean Granahan (The Floating Hospital), Robert Hayes (Community Healthcare Network), Paloma Izquierdo-Hernandez (Urban Health Plan), Dr. Luis Freddy Milano (Community Healthcare Network), and to Amida Care President and CEO and RCHN Community Health Foundation Board member Doug Wirth, who is also featured in the City and State New York’s 2021 Pride Power 100 for his leadership in the fight against HIV/AIDS. Bobby Watts, CEO, National Health Care for the Homeless Council, who is a member of the White House COVID-19 Health Equity Task Force, and also serves on the Foundation’s Board of Directors is recognized as one of Biden’s Policy Pros: Names to Know in Covid relief, the economy, equity and climate.
__________________________________________________________________________________________________________________________
What a Great Run it Has Been! A Look at Our Work and Partners




